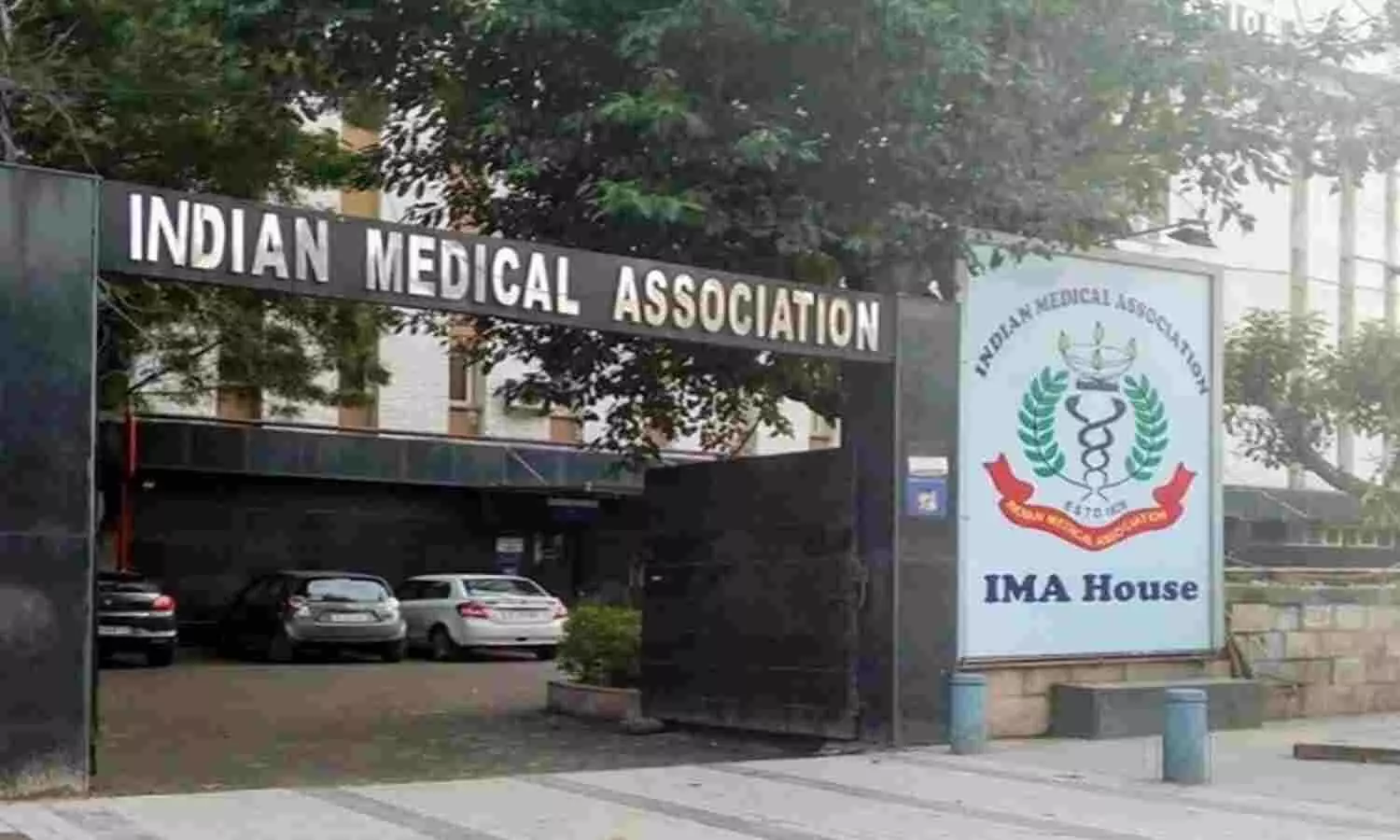
The Indian Medical Association (IMA) has voiced concern regarding a recent directive from the National Medical Council (NMC), which states that doctors must exclusively prescribe generic medications.

Source: Money Control
The IMA has put forth a request to postpone the implementation of this regulation in order to facilitate broader discussions. Furthermore, they have emphasized the need for prompt and significant involvement from both the government and the NMC to address the situation.
Source: Medical Dialogs
Why NMCA made prescription of generic medicines mandatory:
Under the recently introduced guidelines by the National Medical Council (NMC), doctors are now compelled to prescribe generic medications as a mandatory practice. Failure to adhere to this directive could result in penalties, including the suspension of their practicing license for a specified duration.
These regulations, outlined in the “Regulations relating to Professional Conduct of Registered Medical Practitioners,” also emphasize the avoidance of prescribing branded generic drugs. This shift underscores the NMC’s intent to promote the use of generic medicines and curtail the preference for brand-name alternatives within the medical field.

Source: India Times
As detailed in the regulations issued on August 2nd, the document emphasizes the substantial contribution of out-of-pocket expenditure on medications to India’s overall healthcare spending. Citing a significant price disparity, the regulations highlight that generic medicines are notably more cost-effective, ranging from 30% to 80% cheaper than their branded counterparts.
The inherent potential of prescribing generic medications is underscored, with the explicit objective of reducing healthcare expenses and enhancing accessibility to high-quality medical care. Within the framework of these guidelines, the NMC defines generic drugs as equivalent to brand or reference-listed products in various critical aspects such as dosage form, strength, route of administration, quality, performance characteristics, and intended usage.

Source: India Times
What are generic medicines:
The USFDA defines a generic drug as a medication designed to match an existing brand-name drug in various aspects, including dosage form, safety, strength, administration method, quality, performance attributes, and intended purpose.
Despite this, the attempt to enforce an exclusive prescription of generic medicines is met with resistance from the medical community. The Indian Medical Association (IMA) has likened this initiative to operating trains without tracks, emphasizing its urgency. The IMA expresses deep concern over the mandated regulation, asserting that it directly impacts patient care and safety. In a statement, the IMA highlights the need for genuine promotion of generic drugs and compares the current approach by the NMC to running trains without tracks, suggesting an inherent lack of proper guidance and structure in the generics promotion effort.

Source: News9live
Why are generic medicines not the same as branded drugs:
A critical concern raised by medical professionals and health experts regarding generics pertains to their quality. Pharmaceutical companies undergo rigorous stages of quality and safety evaluations during the invention of drugs, leading to approval and often the acquisition of patents.
However, when the patent expires, other pharmaceutical companies gain the right to produce the same medication using the identical formulation, thus classifying it as a generic drug. Unlike the original inventors who invest in extensive research and development (R&D), non-patented pharma companies are able to offer these drugs at a lower price, as they are not burdened with R&D expenses.
Q. What are #genericmedicines and how India became the #pharmacyoftheworld?
Ans. Generic medicines are copies of brand-name drugs that have been approved by the #FDA for safety and efficacy. They are typically much cheaper than brand-name drugs, and they work just as well.… pic.twitter.com/NnEWngkZvd
— Raj Malhotra (@Rajmalhotrachd) August 16, 2023
Moreover, generic drug manufacturers are not required to conduct trials to demonstrate the drug’s efficacy, as they adhere to the original formulation. A distinctive concern arises due to the regulatory landscape in India, where bioequivalence studies are not mandatory prior to obtaining a license for drug distribution, setting it apart from global regulatory practices. This omission raises questions about the equivalence of generic drugs in terms of quantity, quality, and impurities in comparison to their patented counterparts.
What is the hullabaloo about, then?
If all are brands, writing the generic name only shifts the brand choice from Dr to the chemist.
Does not address either the price or the quality issue.
While they are at it, how about shifting the clinical responsibility also to the chemist? https://t.co/rhY94o8Qed— Soumitra Pathare 🌻 সৌমিত্র சௌமித்ரா பாடாரே (@netshrink) August 15, 2023
Notably, Soumitra Pathare, the Director of the Centre for Mental Health Law & Policy, has highlighted this issue in a series of tweets, highlighting the reliance on the word of Indian pharmaceutical companies, lacking substantial data, to affirm the comparability of the generic drugs they offer to the original patented versions.
Also Read:
Dark Truth Revealed About Paracetamol: Fever Killer Or Liver Killer?